1. Blockchain-based EHR systems emerge
Although significant efforts have been made to make health records interoperable, there often have been security-related risks associated with these efforts. Recent ransomware attacks and cybersecurity breaches have further added to the concerns over the security of health data.
The use of blockchain technologies for documenting and transferring patient data is being considered as one of the solutions for achieving interoperability and overcoming data exchange issues.
"This will necessarily require disruptive design changes in EHR architecture, and some vendors are already exploring blockchain to be the new model for ensuring the interoperability of patient information among different institutions," Dhawal Thakur, healthcare research lead at research firm MarketsandMarkets said. "In 2018, several more vendors will be putting forth blockchain-based EHR solutions as one of the major areas of innovation or technological transition."
2. Security gains a seat in the boardroom
"CISOs need to help executives and board members understand the ROI, cost-benefit analysis and security program tradeoffs by articulating the business risk versus business value," said Brendan O'Connor, security chief technology officer at Service Now, an IT and security consulting firm.
In the coming year, the healthcare industry will see infosec leaders doing more to present their security concepts and programs in business terms, O'Connor said. Talking about securing data is one thing, but demonstrating the value that security offers the organization is something else.
"This will eventually apply to every aspect of the business, but most immediately applies to regulatory compliance, potential lost revenue, customer relationships, legal liability, competition, intellectual property, stockholder loyalty and brand protection," he said. "The boardroom needs to take a step toward security, and security operations need to take two steps toward the boardroom."
3. Healthcare continues its move to the cloud
Provider organizations are quickly discovering that cloud-based systems can be more secure and more sophisticated than on-premises technologies. Put another way: Healthcare organizations are discovering that cloud-based systems may very well be the future.
"They are often more secure than traditional on-premises solutions - Amazon Web Services can create a more secure environment than a healthcare organization with limited IT staff and security experience," said Mark LaRow, CEO of Verato, a patient matching technology vendor. "And they can offer a dramatically lower total cost of ownership than traditional on-premises solutions by eliminating maintenance fees and upgrade costs, and by requiring much less effort to install and operate."
4. Digital health and Big Data translate into real health outcomes
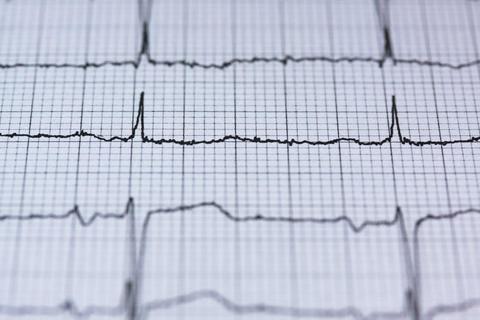
"Big Data analytics is set to bring about significant advancements in terms of creating a more technology-enabled approach to develop preventive medicine and personalized treatment pathways," said Thakur of MarketsandMarkets. "The availability of a significant volume of information from digital health devices used by patients or individuals on a daily basis is further strengthening this approach."
With the help of analytics, technologies are reaching a point where it will be possible to predict when and why patients will be rehospitalized, and what will be the expected therapy response and recovery time, Thakur said. From a provider point of view, this will translate into improved reimbursements, regulatory compliance, better health outcomes and operational optimization.
"2018 is set to bring exciting outcomes for digital health and Big Data analytics," Thakur said. "With the transition toward a more passive way of monitoring patient health, physicians will increasingly start prescribing IoT-enabled devices for real-time access to vital signs. Technological enhancements will keep pushing specialized devices for monitoring specific patient biometrics into the market, and IoT devices, coupled with Big Data analytics, will form the basis of virtual care or telehealth services."
5. A security breach affects someone's physical well-being
There is a difference between information security and physical security. The breaches that plague organizations today are primarily information security violations. While painful, having credit card information, a social security number or personal digital information stolen does not result in physical harm to the victim.
"In 2018, we will see a breach impact our physical, personal lives," said O'Connor of Service Now. "It might be a medical device or wearable that is hacked and remotely controlled. Perhaps it will be an industrial IoT device or self-driving car that gets compromised. Or something closer to home, like smart garage doors. The impact of such an attack will force government, business and individuals to take a closer look at the security of our infrastructure."
6. AI and the IoT will begin to improve workforce shortages
Healthcare faces complex workforce surpluses and shortages leading up to 2030, particularly with clinicians who will be crucial in navigating the shift from volume to value, Forrester Research said. But healthcare is uniquely positioned to work side by side with computers to optimize an already unbalanced workforce.
Healthcare digital business strategy professionals will invest in AI technologies, business processes and the Internet of Things to help close skills and labor gaps for specific use-cases, according to the Forrester Research report, "Predictions 2018: Digital Will Disrupt Siloed Healthcare Ecosystems."
Source: Healthcare IT News (View full article)