January 2018 Archives
Jan 10, 2018
The future of the ACA was uncertain throughout 2017, and though President Trump recently took steps to dismantle it via executive order, it remains unclear how, and how soon, his actions will affect healthcare.
It should come as no surprise then that, according to Managed Healthcare Executive's 2017 State of the Industry Survey, government requirements and mandates top your list of challenges. In addition, shifting toward value-based care is high on the list, as is using big data to improve healthcare quality and reduce healthcare costs. Controlling rising specialty drug costs is another big burden.
The survey's findings, based on more than 300 responses received during the third quarter of the year, show the biggest challenges that executives at health systems, health plans, pharmacy benefit organizations, and more are facing and anticipate continuing to face next year. Here's a closer look at the survey results, and what industry experts advise organizations to do to overcome these challenges.
Challenge #1: Complying with government requirements and mandates
Adhering to government requirements and mandates tops all challenges, at a whopping 34%. This is down just a tad from last year's survey, when it was 36%. "The big question on everyone's mind is, what will become of the ACA?" says Zach Hafner, national partner, consulting, Advisory Board, a healthcare consultancy firm. "Addressing this question at this point requires more precision because the government is deconstructing the broader legislation and taking on various components of it."
President Trump recently announced he will end cost sharing reduction payments to insurers, and he scaled back requirements for employers to provide birth control as part of health coverage for employees. "But these aren't the only potential targets; pre-existing conditions, mandatory insurance coverage, minimum policy inclusions, Medicaid expansion, and selling health insurance policies across state lines are all potential pressure points as the law is revisited and revised in the coming year," Hafner says.
Challenge #2: Implementing value-based reimbursement
Placing second among survey respondents' biggest challenges is implementing value-based reimbursement, which received 22% of responses. Overall, more than half of survey participants, 56%, either have not yet started value-based payment initiatives or have only started a few initiatives. This does show some progress, as last year nearly 70% of survey respondents said they had not yet started or only had a few initiatives started.
Hafner says one reason organizations struggle in this area is that today's fee-for-service system is not well aligned to deliver true value-based care, and for most provider and payer participants, most business remains fee-for-service. The country continues to tolerate fee-for-service and annual reimbursement increases. "Until that changes, we can't really expect payers and providers to make the change," he says.
Secondly, delivering value-based care requires different infrastructure, work flow, and information than what has been in place historically, all of which require investment. Some examples of this include physicians needing to collaborate, integrating clinical and financial data, and having the capability to evaluate, negotiate, and administer risk-based contracting arrangements. To date, the return on such investments has been elusive.
Thirdly, even after a decision is made to move a business model to value-based pay, data and insights needed are not easy to obtain and often considerable lag time occurs when compiling it.
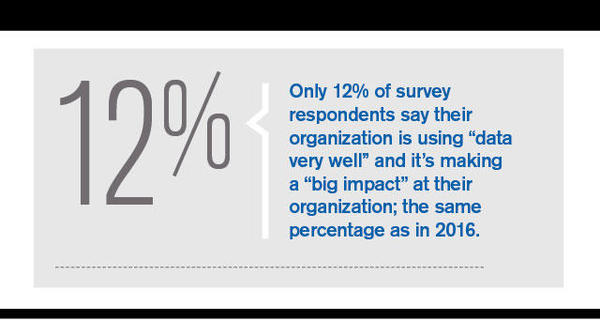
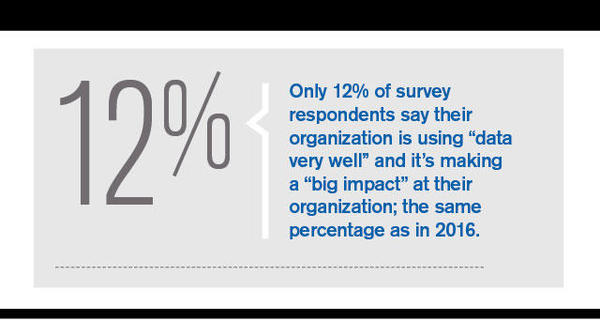
Challenge #3: Using big data to improve quality and reduce costs
This is a third major challenge facing organizations. Only 12% of survey respondents say their organization is excelling in this area; the same percentage as in the 2016 survey. Forty six percent of 2017 survey respondents say they "have come a long way" in this area, but that they have a lot more work to do in this space. That's up from 39% last year.
Shroff sees two main big data challenges. Although more healthcare data is being generated, the data is scattered across multiple entities--payers, providers, and patients. There is no such thing as a single "source of truth" for healthcare data.
"When patients jump between different health plans or providers, the data doesn't follow the patient," he says. "This, coupled with the lack of interoperability between entities, makes it difficult to harness data-driven insights."
Secondly, most organizations lack the proper technology to manage or capitalize on the vast amount of information they possess. Healthcare data comes in various formats and sources--clinical data from EHRs, billing data from claims, patient enrollment or registration data, as well as self-reported patient data, Shroff says. To truly unlock the power of big data, organizations need a technology infrastructure that retrieves, stores, and analyzes various sources of data at scale.
Health plans and systems have the same challenge--getting access to the data that the other has. "A health system has access to the patient's most in-depth clinical data, but it's often limited to the specific episode of care that was provided at that system," Shroff says. "When a patient visits other provider groups or hospitals, it's the patient's responsibility to recall the care that was provided at the other settings." On the other hand, health plans are aware of every encounter that a patient has, regardless of which system they visit. However, their depth of knowledge is limited to the billing data sent from the systems. "Having both entities share their respective data would most likely result in better quality and cost savings, but organizations are simply not set up to do so in today's world."
Source: Modern Medicine Network (View full article)
Dan Corcoran | Permalink | Comments (0)
Jan 10, 2018
We are elbow-deep in an age of disruptive technologies that aren't just buzzwords any longer, but are entering into our health systems and every day clinical care.
The University of Pittsburgh Medical Center, for example, an innovator in using analytics, has recently also begun harnessing artificial intelligence to improve care.
The health system has developed AI-based algorithms used on its more than 27 petabytes of data to define patient subpopulations -- those with congestive heart failure or asthma, for instance -- to target interventions to those groups. It's developed algorithms using electronic health record data to predict patient decline in hospitals.
In operations, it uses AI to predict which patients won't show or cancel appointments within 24 hours, an effort to determine the availability of same-day appointments.
Machine learning and artificial intelligence are among the disruptive technologies research firm IDC highlights in its Worldwide Health Industry 2018 Predictions report. Others include: the Internet of Things, 3-D printing, next-generation security, augmented reality, virtual reality and blockchain.
New Health Technologies Mean New Vulnerabilities
Securing the proliferation of data from these technologies will provide an immense challenge for healthcare organizations, according to Lynne Dunbrack, research vice president for IDC Health Insights.
With more data, there's a bigger attack surface, she points out.
"The data sets are more robust now. They include clinical data, financial data, other identifying data of the social demographic. The personally identifiable data can then be used for medical identity theft. It all makes healthcare data that much more attractive for cybercriminals to attack healthcare, which is considered a soft target compared with other industries that invested earlier in security technology," she says.
The explosion of IoT devices and networked medical devices are the biggest security threats among the emerging disruptive technologies in the view of Christopher Frenz, director of infrastructure at Interfaith Medical Center in New York. He wrote the Open Web Application Security Project's (OWASP) report on medical device deployment.
Frenz points to the WannaCry ransomware attack, which affected some radiology equipment, as the most chilling example.
"WannaCry showed it's not just a patient information issue, but a patient safety issue as well," he says. "This creates a whole new and wholly unacceptable meaning for denial of service."
Holistic Security Can Offer Health Systems Safe Harbor
Among the IDC predictions: By 2021, the world will have seen its first $100 million class-action lawsuit against a medical device manufacturer for negligence because of a cyberattack causing the death of more than 25 people connected to networked medical devices while hospitalized.
The security implications of new technologies must be evaluated individually, according to John Houston, vice president of privacy and information security at UPMC. It has a structured program to do that, whether it be artificial intelligence, Google Glass or any other emerging technology, he says.
"Any platform is going to have specific components that raise specific considerations from a security perspective, especially around how it's going to be used in a hospital setting," Houston says.
He considers the dramatic shift to the cloud one of healthcare's greatest security challenges, since the data no longer remains under the organization's control. And sensitive data is being pushed out in all sorts of new ways to patients' devices and to physicians who may be vacationing in other parts of the world.
"I really have to think about how data is stored and delivered all over the planet. ... It really is a problem of scale and where that data resides," Houston says.
Security must be part of the conversation from the early design stages of any new project.
"You need to think about how it's going to be used, how it's going to be accessible, how data is going to be managed," he said.
Healthcare's approach to security traditionally has been comparable to the way preschoolers play soccer, according to Dunbrack -- everyone goes after the ball at the same time. When there are phishing attacks, for example, everyone invests in anti-phishing technology.
"You really need to take a holistic view of security," she says, advocating for a layered approach to cyberdefenses.
Every new technology is going to bring new risks, so any good security program is going to involve continuous evaluation and continuous improvement, according to Frenz.
He recommends using zero trust and defense in depth strategies because the traditional firewall approach to security just doesn't work anymore, he claims. Signature-based defenses increasingly are ineffective because the majority of attacks involve malware the systems haven't seen before.
The next-generation security IDC refers to uses AI and machine learning to determine normal system behavior and alerts on aberrations. By allowing only "known good" communications -- the acceptable calls components need to make to do their jobs, for instance -- it relieves organizations from just chasing after the ball.
Source: HealthTech Magazine (View full article)
Dan Corcoran | Permalink | Comments (0)
Jan 8, 2018

While 2017 may be the year in which bitcoin took the investing world by storm, 2018 may be the year when bitcoin's underlying technology, the blockchain, takes the business world by storm. In fact, IBM (NYSE:IBM) CEO Ginni Rometty said earlier this year that, "What the internet did for communications, I think blockchain will do for trusted transactions."
Bitcoin was conceived as a peer-to-peer currency with no central authority, in which the underlying blockchain technology was so transparent and un-alterable that no government entity was needed to govern transactions. That transparency and security is what is so attractive -- and perhaps revolutionary -- to industries such as global finance, shipping, and food safety. Of course, large corporations need a trusted party to run their blockchain networks. With its decades of experience in operating technologies for business, IBM is an early mover in this space.
I was recently afforded the opportunity to hold an exclusive interview with Jerry Cuomo, IBM's vice president of blockchain technologies, to learn more about IBM's active blockchain networks -- some of which are already very large and mature -- as well as the technology behind them. In Part 1 below, we'll go over some of what Cuomo had to say about the high-level picture of what blockchain is and how it is being used already by a variety of industries. In Part 2, I go over what he had to say about how blockchain works in IBM's cloud, how the technology was conceived in the Hyperledger Project, and the current competitive dynamic implementing this open-source technology.
Here are some of the highlights from my conversation with Cuomo. IBM provided the transcript. I edited some of the quotes for clarity.
Blockchain for business
I asked Cuomo to describe from a high-level perspective what blockchain technology is, from IBM's perspective. He said:
I think there are two sides to the coin of blockchain. One is a social phenomenon, but that's powered by a technological phenomenon. And from a social phenomenon, it's really a new way for businesses to interact. Interact in a way that's more direct, and in such a way where trust is distributed across the businesses, to enable the group to achieve more than any of the individual members could achieve.
From that, there's a range of, obviously, more basic cost-saving types of things that a blockchain network could provide to a group of collaborating companies, to a whole new set of business processes. Some that we're conceiving, and some that haven't even been conceived yet. And it's all powered by this distributed ledger technology that is made famous by bitcoin, but not limited to cryptocurrency as a use case.
I then asked him about some of the different blockchains, or "active networks," as the company calls them, and how many of them IBM was currently running.
An active network is something that is a network that has multiple institutions, actively exchanging digital assets of value. So, it's a very simple definition of multiple institutions actively exchanging things of value through a distributed ledger. From that perspective, we're on track this year [2017] to do over 35 of those active networks.
Industry applications
I asked Cuomo and to describe some of the more prominent active networks IBM is managing.
The elder of the group is the Global Finance Network. That's associated with this channel financing network that finances things like parts for computers for institutions assembling or shipping or consuming computer parts. That is about $40 billion per year in capital in that network, and at any given time, there can be up to $100 million in money that is held in dispute. So, you know, I shipped you something. I said I shipped it. You said you haven't received it, but the shipping company said they sent it-- it's not uncommon for that to happen.
A year and a half ago, one of the elder statesmen is this network, where now we have over a dozen of the highest-transacting institutions in this supply chain. There's about 4,000 suppliers and consumers in that network. We only have a small portion of them, but the portion that's responsible for the majority of the interactions. And we're seeing disputes now which were taking on average 44 days now being resolved in under 10 days.
That's the most active of our networks, and part of it is because it's been out for a while. There's several million blocks on the ledger now, representing the transactions that are part of this dispute resolution process.
Source: The Motley Fool (View full article)
Dan Corcoran | Permalink | Comments (2)
Jan 8, 2018
Lots of health systems pay lip service to patient-centric care, but what does that really mean? As healthcare continues its transition to paying for value and outcomes, toward managing wellness rather than treating disease, making the patient an active participant in the process is more important than ever.
Some hospitals and health systems are better at doing this that others. Certainly many have worked in earnest these past few years to do it well. And no question, there's a wide array of different tips, tricks and tools to getting patient engagement right.
At the Patient Engagement & Experience Summit, which takes place Monday, March 5, at HIMSS18 in Las Vegas, experts from across healthcare - clinicians, technologists, patient advocates, chief experience officers and others - will gather for a day-long event to compare notes and share success stories and best practices for getting patient populations more involved with and attentive to their own healthcare.
Just as important, some speakers will focus on the patient experience - ensuring that care delivery in hospitals, physician practices and post-acute care settings is respectful and responsive to specific needs - perhaps even enjoyable.
Both engagement and experience are necessary in the era of accountable care, after all. The former is key to care coordination, chronic disease management, medication adherence and reductions in readmissions - all critical for value-based reimbursement. The latter can be the difference in creating a competitive edge compared with the hospital across town.
The Patient Engagement & Experience Summit, co-presented by HIMSS and the Cleveland Clinic, will convene providers, payers, policymakers and others to offer well-honed advice on the technologies and strategies that can help improve on both counts.
The day's events will be emceed by Adrienne Boissy, chief experience officer at Cleveland Clinic Health System.
Other speakers will include Pracha Eamranond, senior vice president medical affairs and population health at Harvard Medical School's Lawrence General Hospital; Larry
Chu, professor of anesthesiology, perioperative and pain medicine at Stanford; David Asche, executive director of Penn Medicine's Center for Health Care Innovation, and Donald Kosiak, chief medical officer at Leidos.
Source: Healthcare IT News (View full article)
Dan Corcoran | Permalink | Comments (0)
Jan 8, 2018
CFOs rated cost reduction as the most important performance management activity for 2018, according to a new Kaufman Hall survey of senior finance professionals.
Nearly 30 percent chose "identifying and managing cost-reduction initiatives" as the most important performance management function for their organizations, from a list of five choices, according to the 2018 CFO Outlook: Performance Management Trends and Priorities in Healthcare.
The other four priorities, in order, are improving performance reporting to operational leaders (25.8 percent); predicting and managing the impact of changing payment models (18.1 percent); developing more integrated and planning processes across financial planning and strategic capital allocation (16.3 percent); and leveraging rolling forecasting as part of a more continuous planning and financial performance monitoring process (10.7 percent).
Most CFOs, however, also said they have limited confidence in their organization's ability to manage the financial impact of evolving business conditions. Only 15 percent said their organizations are "very prepared" to manage evolving payment and delivery models with current financial planning processes and tools.
Seventy-percent said they have cost measurement tools that are too simplistic or provide inaccurate data that can't be trusted or have no tools in place at all, according to the survey of senior finance executives at 350-plus hospitals and health systems.
Fifty-six percent of CFOs and executives said their organizations lack access to clean, consistent, and trusted data, while ninety-percent think their hospitals should be doing more to leverage financial and operational data to inform strategic decisions.
CFOs said long budgeting cycles are preventing value-added analysis by finance teams. Sixty-nine percent have a budget process that takes more than three months from initial rollout to board presentation. For 9 percent of these organizations, the process takes more than six months.
The survey addresses the rapidly changing healthcare business environment, and the growing role and importance of the CFO function to inform strategic business decisions that will impact long-term success, according to consulting firm Kaufman Hall.
Source: Healthcare Finance (View full article)
Dan Corcoran | Permalink | Comments (0)
Jan 8, 2018
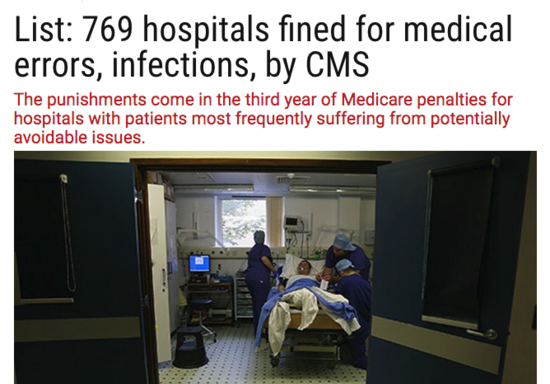
The federal government has cut payments to 769 hospitals with high rates of patient injuries, for the first time counting the spread of antibiotic-resistant germs in assessing penalties.
The punishments come in the third year of Medicare penalties for hospitals with patients most frequently suffering from potentially avoidable complications, including various types of infections, blood clots, bed sores and falls. This year the government also examined the prevalence of two types of bacteria resistant to drugs.
Based on rates of all these complications, the hospitals identified by federal officials this week will lose 1 percent of all Medicare payments for a year -- with that time frame beginning this past October. While the government did not release the dollar amount of the penalties, they will exceed a million dollars for many larger hospitals. In total, hospitals will lose about $430 million, 18 percent more than they lost last year, according to an estimate from the Association of American Medical Colleges.
The reductions apply not only to patient stays but also will reduce the amount of money hospitals get to teach medical residents and care for low-income people.
Specialized hospitals, such as those that treat psychiatric patients, veterans and children, are exempted from the penalties, as are hospitals with the "critical access" designation for being the only provider in an area. Of the remaining hospitals, the Affordable Care Act requires that Medicare penalize the 25 percent that perform the worst on these measures, even if they have reduced infection rates from previous years.
That inflexible quota is one objection the hospital industry has with the penalties. In addition, many hospitals complain that they are penalized because of their vigilance in detecting infections, even ones that do not cause any symptoms in patients. Academic medical centers in particular have been frequently punished.
"The HAC penalty payment program is regarded as rather arbitrary, so other than people getting upset when they incur a penalty, it is not in and of itself changing behavior," said Nancy Foster, vice president for quality and patient safety at the American Hospital Association.
Federal records show that 347 hospitals penalized last year will not have payments reduced because their performance was better than others. Those include Harbor-UCLA Medical Center in Los Angeles, the Johns Hopkins Hospital in Baltimore and the University of Tennessee Medical Center in Knoxville.
Source: Healthcare Finance (View full article)
Dan Corcoran | Permalink | Comments (0)